My Specialty
Associate Professor and PNP, Nancy Pike, UCLA School of Nursing
Training APRNs to fill the primary care gap
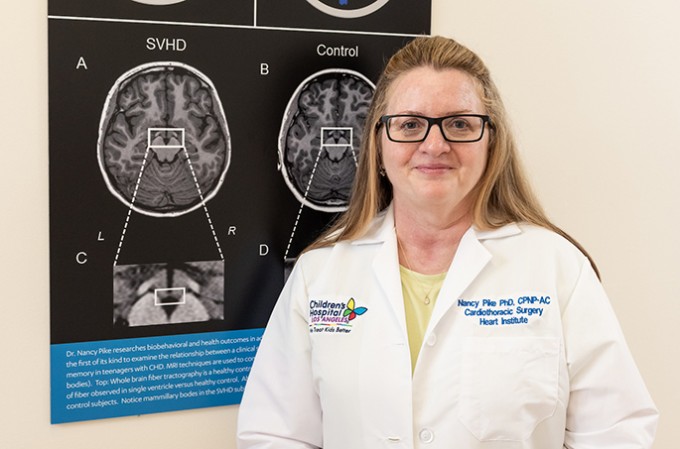
Nancy Pike, RN, Ph.D., CPNP-AC/PC, FAAN
Associate Professor and Pediatric Nurse Practitioner
UCLA School of Nursing
Please tell us about your nursing career journey.
I’ve been a nurse for 34 years. I graduated with my BSN from Penn State University in 1985. My first nursing job was in an adult med/surg ICU at Hershey Medical Center, taking care of mostly postoperative cardiac surgery patients. Not long after I started, my manager asked if I wanted to learn how to take care of pediatric cardiac surgery patients. That was my first experience taking care of children and I loved it. I wanted to earn my MSN, but there were only a few cardiopulmonary MSN programs in the U.S. and UCLA had one of them. So, I moved to California, graduating in 1993.
My next clinical position was at Stanford at the Lucile Packard Children’s Hospital. It became apparent that I needed to medically manage patients, so I did a post-master’s nurse practitioner certification at UCSF.
In 2003, I returned to Southern California to pursue a Ph.D. at UCLA. I continued to work part-time as an NP in pediatric cardiac surgery at Children’s Hospital Los Angeles. I completed my Ph.D. in 2007. Around 2009, I transitioned to academia and took a faculty position at UCLA School of Nursing.
Are you practicing clinically at this time?
I still practice per diem as a pediatric nurse practitioner (PNP) at Children’s Hospital Los Angeles. I enjoy that I can still engage in clinical work while being an educator. It enhances my teaching and keeps me in touch with the concerns of patients living with congenital heart disease.
Tell us about your position at UCLA.
Primarily, I teach in the PNP program and have an NIH-funded research program focusing on adolescents with congenital heart disease, in particular single ventricle heart disease. I’m looking at structural changes in the brain, cerebral blood flow and neurocognitive outcomes in teenagers who have had multiple open-heart surgeries at a young age. My goal is to develop and test interventions that can improve cognitive deficits and the patient’s future self-care ability.
What changes are you seeing in the education of advanced practice nurses?
Over the past decade, I’ve seen the growing need for PNPs in the inpatient and acute settings. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) imposed medical resident hour restrictions, which were updated again in 2010. Coupled with a shortage of primary care physicians in many communities, this has led to a need for highly skilled nurse practitioners — not just PNPs — in both acute and primary care.



