My Specialty
Clinical Navigator Perinatal Services, Michael Russo, Henry Mayo
Improving processes and systems while empowering the nursing team
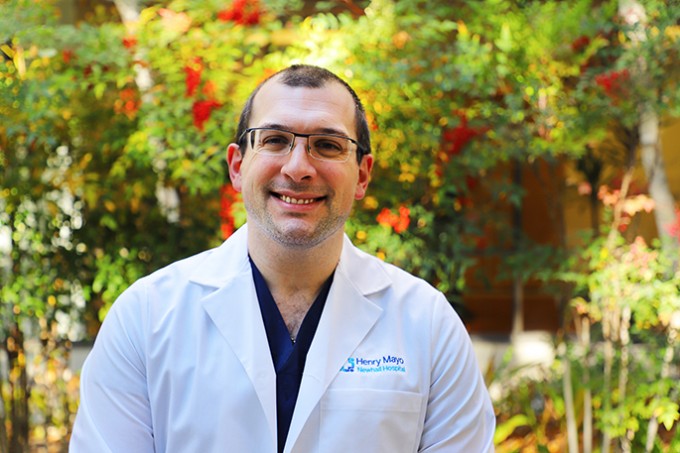
Michael Russo, RNC-NIC, MSN, CLC
NICU Clinical Navigator Perinatal Services
Henry Mayo Newhall Hospital, Valencia
Please describe the trajectory of your nursing career.
I began my career in 2012 by finding an internship program in pediatrics at Children’s Hospital of Orange County. I floated a lot to the NICU there and fell in love with it. In 2013, I was trained as a staff nurse in the NICU at Cedars-Sinai. While working the night shift there, I earned my master’s in nursing education, which led me to the career path I’m currently traveling.
Why did you choose pediatrics?
Both the relationships with the families and advocating for this very special population who can’t speak for themselves have always appealed to my heart. When I was in school, I knew pediatrics was for me. I so enjoy talking with the kids, helping them through rough procedures and counseling and supporting the parents. My ability to connect and ease worries took on a new level of importance when I started working in the NICU.
What is your position at Henry Mayo and what does it entail?
I’m the clinical navigator of the NICU, which along with L&D and postpartum comprise the perinatal department. As clinical navigator, I’m responsible for connecting with staff and assessing their skills over time. I also round on parents and families to troubleshoot any potential patient experience issues.
Being a navigator is an umbrella position that includes process improvement, troubleshooting clinical issues, unit-based issues, clinical skills assessments, systems analysis and collaboration with many other units. A navigator has so many things to do that we can’t just be put in a single box.
In order to navigate the realm of the NICU, you must have space, time and resources. I feel I have a lot of room to be creative and flexible in this position, whether it’s doing data entry, researching patients, pulling information for chart audit or creating education for the unit.
How does the clinical navigator support the NICU nurses?
I work very closely with the clinical manager of the NICU, but my role is definitely advisory. I make sure my nurses are heard, acknowledged and respected. I empower them to use their voices to speak up if there are issues in the unit or if a process needs improvement.
It could be as simple as improving and/or optimizing the documentation in the electronic medical record, or something more complex, like examining evidence-based research about a pathophysiologic process and sharing that knowledge with the nurses.












