Feature
The Gruesome Origins of Blood Pressure Measurment
Imagine if you had to puncture an artery every time you needed to take a patient’s blood pressure!
Checking a patient’s pulse has been an important diagnostic technique for thousands of years. However, measuring blood pressure is a more recent development.
Cruel Experiments
Our modern conception of the circulatory system stems from a 1628 book by English physician William Harvey. He argued that the body contained a finite amount of blood which circulated due to the action of the heart. This was a surprisingly controversial idea at the time, but it set the stage for the actual measurement of blood pressure.
A century after Harvey’s book, English scientist Stephen Hales conducted a series of gruesome experiments to measure the blood pressure of live animals, beginning with an unfortunate mare.
As Hales wrote in 1733:
Having laid open the left crural artery about three inches from her belly, I inserted into it a brass pipe. To that I fixed a glass tube which was nine feet in length. Untying the ligature of the artery, the blood rose in the tube 8 feet 3 inches perpendicular above the level of the left ventricle of the heart.
This dramatic demonstration wasn’t exactly useful for medical practice — none of Hales’ subjects survived these ghastly tests!
Puncturing the Artery
A century after Hales’ live animal experiments, Jean Léonard Marie Poiseuille wrote his dissertation on measuring arterial blood pressure. His procedure involved inserting a cannula into the artery and measuring the pressure with a mercury manometer.
This was less lethal than the Hales experiments, but puncturing the artery was still very risky.
Mercury in a Glass Tube
The first noninvasive attempt came in 1833, when Jules Herisson created a device using a bulb full of mercury connected to a glass tube. The user pressed the bulb against the radial artery until the pulse was obliterated. The height of the mercury in the tube showed the systolic pressure, much like a mercury thermometer.
Although Herisson published his findings, he didn’t include any actual readings, and his instrument was so crude that the results probably wouldn’t have been very accurate.
Weights and Screws
The next generation of devices were given Greek names and incorporated new techniques. Carl Ludwig developed a more elaborate version of Poiseulle’s device, which would record its readings on a revolving drum. Ludwig called this a kymograph, from the Greek “kymo” (wave) and “graph” (writer).
Karl von Vierodt applied the same idea to an invention he called a sphygmograph, from the Greek “sphygmos” (pulse). This cumbersome apparatus placed a weighted pad over the radial artery and traced the pattern of the patient’s pulse on the rotating drum. By adding more weights until the pulse was obliterated, the user could estimate the patient’s systolic blood pressure.
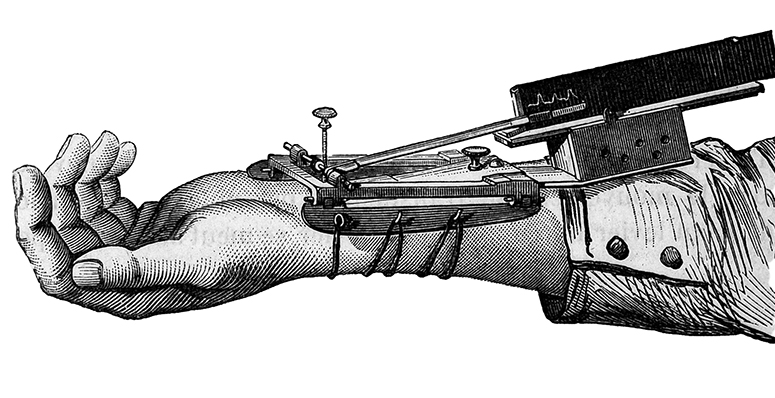
In the 1860s and 1870s, Étienne Jules Marey and others created smaller, easier-to-use sphygmographs that strapped to the subject’s wrist and used an adjustable screw rather than weights to increase the pressure on the artery. (see the illustration on page 18).
These were really the first blood pressure measuring tools that were actually practical for real clinical use — and unlike arterial puncture, they were unlikely to kill the patient!
Some technophiles of the time saw such devices as part of an exciting new scientific revolution in medical care, but the truth was that many of these contraptions were still too cumbersome and complicated for routine use, and the readings often weren’t very accurate.
Many clinicians weren’t convinced that these gadgets were any better than simply measuring the pulse with a finger.
More Accurate Readings
In 1880, Samuel Siegfried Karl Ritter von Basch came up with a much improved new instrument with the tongue-twisting name of sphygmomanometer (pulse-pressure meter).
It consisted of a water-filled flexible rubber bulb, called a pelotte, attached to the end of a glass tube containing mercury.
This was basically a better version of Herrison’s crude device from the 1830s, and it was used in the same way (pressing the pelotte against the radial artery to obliterate the pulse, causing the water to displace the mercury into the tube). However, its readings were vastly more accurate.
The inflatable Cuff
Italian physician Scipione Riva-Rocci looked at the latest sphygmomanometers and devised a new version all nurses will recognize: the inflatable blood pressure cuff. This applied pressure to the brachial artery from all sides rather than just one, giving more reliable, uniform results.
There was still one serious flaw: Early cuffs were too narrow, which could apply too much pressure to the artery and give inaccurate readings. Later evolutions widened the cuffs to about 4¾ inches.
Faint Tapping Sounds
Although these latest sphygmomanometers could now accurately measure systolic pressure, determining diastolic pressure remained difficult.
However, Russian surgeon Nikolai Sergeivich Korotkoff presented a short paper in 1905, describing the faint tapping sounds that could be heard through a stethoscope as pressure in the cuff decreased, which Korotkoff believed marked the points of systolic and diastolic pressure.
After additional studies confirmed his theory, the Korotkoff auscultatory method was widely adopted in the years leading up to World War II.
Combining this technique with the inflatable cuff finally established blood pressure measurement as an accurate, reliable, noninvasive clinical assessment, which is now a basic skill for every nurse.
AARON SEVERSON is the associate editor of Working Nurse.
In this Article: technology


