Feature
When Care Meets Conflict
Strategies to help keep nurses safe from workplace violence
As nurses, you have an amazing passion and a commitment to providing the highest quality of care for your patients. Yet, for more reasons than we have space to list, aggressive and violent behavior of patients and others can make it extremely difficult for you to do your job safely.
Our company, KLA Risk Consulting, has a division dedicated to workplace violence in hospitals and ambulatory care. This article offers insights drawn from our extensive work in this area.
Reducing injuries due to workplace violence requires doing some things differently. Employers play a crucial role in creating safer workplaces, but you can do quite a bit too.
Here are five tips for individual nurses, with some examples drawn from real incidents.
1. Do not accept that violence is “just part of the job.”
 A patient under the influence of alcohol pointed at his nurse and yelled obscenities. Once he was close enough, he grabbed the nurse’s wrist and exclaimed, “If you touch me, I’ll break your arm.” The nurse freed his wrist, told the patient to behave himself, and went on to the next patient. He shrugged off the assault as “just part of the job.”
A patient under the influence of alcohol pointed at his nurse and yelled obscenities. Once he was close enough, he grabbed the nurse’s wrist and exclaimed, “If you touch me, I’ll break your arm.” The nurse freed his wrist, told the patient to behave himself, and went on to the next patient. He shrugged off the assault as “just part of the job.”
If you accept that workplace violence is just part of being a nurse, you may find yourself dismissing or ignoring it. You don’t have to. There’s nothing in your job description or any hospital policy that says you must tolerate assault. Further, accepting that violence is “part of the job” helps to perpetuate it.
2. Review your hospital’s policies and procedures.
One of the reasons nurses accept assault while on duty is that they misunderstand their hospital’s policies, or the policies are unclear.
For example, one of the most common workplace violence scenarios is when nurses attempt to keep a patient from leaving the hospital, fearing they will be reprimanded or even fired for allowing the patient to leave.
This is rarely true: Elopement and “against medical advice” policies don’t require that you put yourself at risk to keep a patient from leaving. This is why it’s important to familiarize yourself with your institution’s official policies.
If you have questions, get answers — and if you feel the current policies put you or your coworkers at risk, speak up to your nursing leadership, safety committee, or shared governance council.
3. Learn to recognize and watch for agitation.
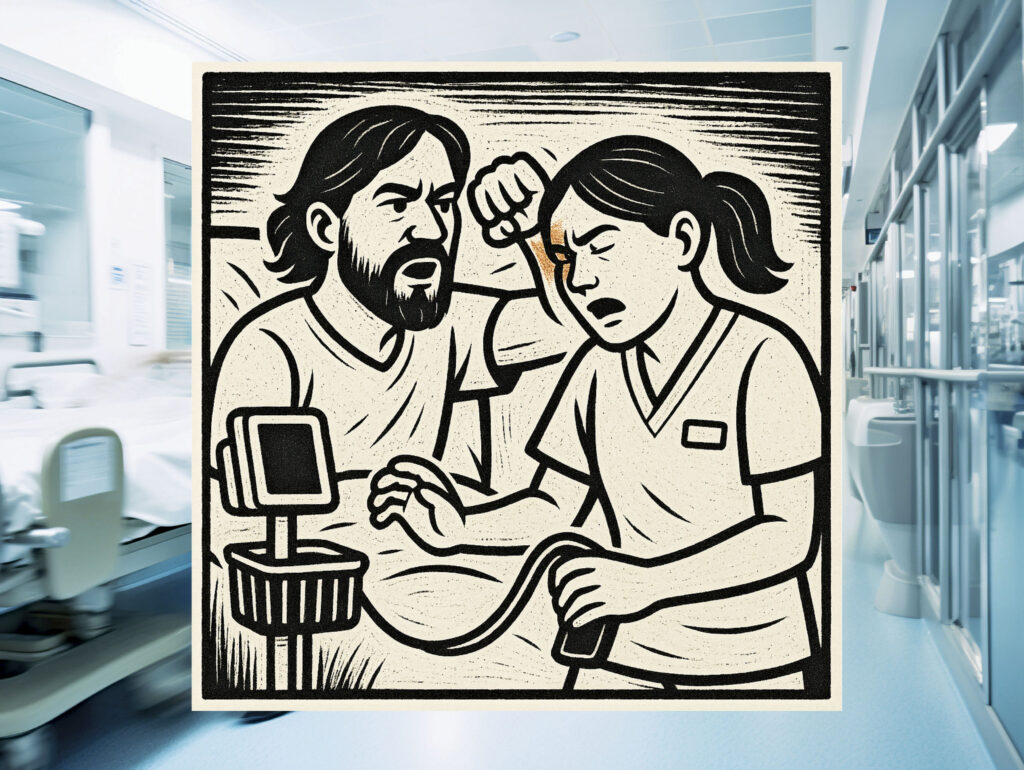
 A nurse entered a patient’s room to check vitals. The patient expressed frustration at being awakened “every five minutes” and demanded, “Can’t you all come in at once?” The nurse rolled her equipment to the bedside and said, “I’m just going to quickly get your vitals.” When she reached down to pick up the blood pressure cuff, he punched her in the head.
A nurse entered a patient’s room to check vitals. The patient expressed frustration at being awakened “every five minutes” and demanded, “Can’t you all come in at once?” The nurse rolled her equipment to the bedside and said, “I’m just going to quickly get your vitals.” When she reached down to pick up the blood pressure cuff, he punched her in the head.
There are a lot of patient aggression risk factors to keep track of, but you can make it easier by adopting the mindset that anyone near you has the potential to assault you. That’s not paranoia — that’s reality.
Since it’s hard to be a nurse without coming into contact with people, your goal is to recognize any change of behavior that indicates agitation, which is a precursor to aggression, and a sign that your safety is at risk.
Agitation is a symptom, but the underlying causes can be almost anything. In the above example, the patient was upset at being woken up, which escalated when the nurse continued what she was doing without acknowledging his frustration.
This is why it is important to recognize agitation before it escalates. Then, you can gain distance and de-escalate the situation until it is safe for you to continue providing care.
Once you resume care, remain alert for any change in behavior that indicates that the patient is becoming angry again, whether it’s for the same reason or for something else.
4. Listen to your intuition.
 A nurse was preparing to draw blood from a patient while the patient’s father stood at the other side of the bed. Something about how the patient was talking gave the nurse the vague feeling that something was not right. Just as she turned her head away from the patient, he punched her in the back of the head. Her rolling stool shifted due to the impact, and she fell and hit her head against the wall, temporarily blinding her.
A nurse was preparing to draw blood from a patient while the patient’s father stood at the other side of the bed. Something about how the patient was talking gave the nurse the vague feeling that something was not right. Just as she turned her head away from the patient, he punched her in the back of the head. Her rolling stool shifted due to the impact, and she fell and hit her head against the wall, temporarily blinding her.
Intuition is the little voice inside us that helps keep us safe. Pay attention and listen to what it is telling you, even if you cannot immediately identify the source of the concern.
If something feels wrong or off, don’t try to talk yourself out of it. If you sense agitation or hostility, or even if you have just “bad vibes” you can’t put your finger on, respond reasonably for your safety.
Remember, you have options: You can gain some distance and begin de-escalation, call for assistance, or back out of the room to seek help. Even if that little voice turns out to be wrong, it’s better to be safe.
5. Make caring for your own emotional and physical health your no. 1 priority.
It’s hard to stay alert and objective or listen to your intuition when you’re exhausted, stressed, anxious, or burned out. Your emotional and physical health are critical to your ability to keep yourself safe at work. Ongoing self-care, at home and at work, is a must.
If you experience a stressful situation with a patient or someone else at work, step away to focus on your own emotional health and well-being. Listen to a favorite song, look at photos of your loved ones, take a walk around the block, do some deep breathing, or whatever helps.
This may be difficult, especially in an emergency department or other fast- paced unit, but doing something, even for just one minute, is better than doing nothing.
Workplace violence in healthcare continues to be a systemic challenge. There has been progress, but more work is needed. Do what you can to protect yourself and stay healthy. We need you!
WORKPLACE VIOLENCE BY THE NUMBERS
- Healthcare workers experienced 14.1 violence-related injuries per 10,000 fulltime workers in 2021–2022 — 5 times the rate of workers in other industries.
—U.S. Bureau of Labor Statistics, 2024 - Nurses experience the highest proportion of physical assaults of any healthcare worker (about 67 percent).
—Chappell & Di Martino study, 2006 - Fifty percent of physical assaults on nurses resulted in injury, including bruises, sprains, and lacerations.
—Minnesota Department of Health study, 2012 - Assaults on nurses rose from 2.59 per 100 nursing personnel in 2022 to 2.71 in 2023, with nearly 17,000 assaults in 2023 — a record high.
—Press Ganey “Safety in Healthcare 2024” report - Over 80 percent of nurses reported at least one type of workplace violence in 2020 during the pandemic.
—National Nurses United (NNU) survey, 2021 - Workplace violence against nurses is significantly under-reported, with estimates suggesting that only 20–30 percent of incidents are formally documented.
—OSHA Guidelines for Preventing Workplace Violence, 2016
KELLY L. AUSTIN, Psy.D., is the vice president of the Hospital Workplace Violence division at KLA Risk Consulting.
In this Article: Workplace Safety