Feature
Wired Hospitals: UCLA Medical Center and High-Fidelity Manikins
Lights! Camera! Action! Septic Shock?
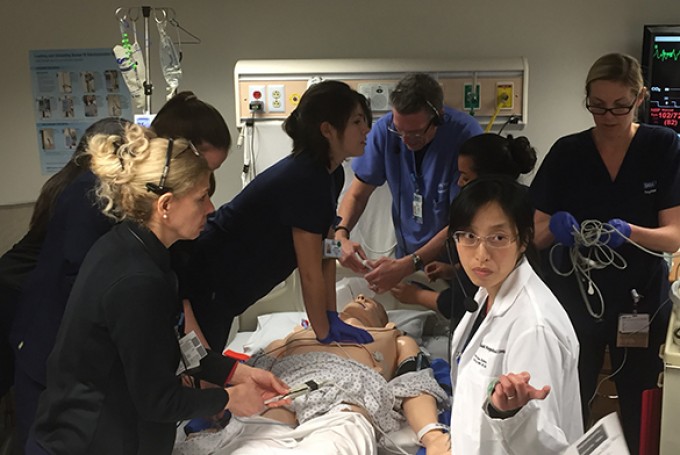
It was bloody. The first big simulation Kenneth M. Miller, RN, MSN, CCRN, CHSE, ran as nursing simulation program coordinator at Ronald Reagan UCLA Medical Center was a hemorrhagic splenectomy in the operating room. He did everything he could to make it look real, draping the patient with a central line and filling 4x4s with blood. “It looked like actually cutting somebody’s abdomen open,” he recalls.
Today, Miller’s program boasts two simulated patient rooms and several high-fidelity manikins, including the Laerdal SimMan 3G, a wireless simulator that can mimic a real adult patient, complete with body fluids, pupillary responses and the ability to convulse.
There’s also Premature Anne, a 25-week-old preemie simulator that can cry, turn blue and replicate abnormal breathing sounds. Miller’s team runs a variety of staff training scenarios: patient falls, atrial fibrillation with chest pain, blood transfusion reaction, infected wounds, septic shock, myocardial infarction — you name it. These exercises are an opportunity to refine teamwork across multiple disciplines in a nonpunitive environment.
Operating Room Theater
Ronald Reagan UCLA Medical Center’s advanced manikin and sim technology is great, but Miller says there is one thing no technology can replicate. “It lacks humanism,” he explains. “We forget there is a patient there.” To address that, Miller has developed an innovative way to bring a human touch to his training simulations: hiring improvisational actors to play the roles of patients.